The human population has always been confronted with pathogens since prehistoric time (Diamond, 2002; Krause, 1992; Dobson & Carper, 1996, Wolfe, et al., 2007). Nevertheless, the occurrence of pathogens and emergence of pandemics have become more frequent since the advent of agricultural revolution around 8000 BC (Diamond, 2002; Diamond, et al., 1997; Dobson & Carper, 1996; McNeill, 1976), and with the beginning of industrialisation in 18th century (Patz, et al., 2004; Neiderud, 2015). Pathogen transmission largely depends upon ecological, environmental and socio-economic conditions of host population (Morens, et al. 2004; Smolinski, et al., 2003; Binder, et al, 1999; Daszak, et al, 2000; Taylor, et al., 2001; Patz, et al., 2004; Weiss & McMichael, 2004; Morse, 1993; Jones, et al., 2008; Dobson & Carper, 1996). The rapidly changing demographic and economic set up, the emerging infectious diseases (EIDs) are causing significant pressure on economies and public health (Morens, et al., 2004; Smolinski, et al., 2003; Binder, et al, 1999). The initiation of sedentary economic lifestyle, increased global movement, and urbanisation and monotones food systems has aggravated the pathogens to become pandemics in the modern times (Dobson & Carter, 1996).
Coronavirus disease (SARS-CoV-2), termed as Covid-19, is an infectious disease caused by a newly discovered coronavirus (WHO, 2020). The genomic analysis revealed that SARS-CoV-2 is phylogenetically associated with SARS viruses, and bats could be the possible primary source of Covid-19 (Chakraborty & Maity, 2020). The socio-economic contexts have contributed to the shifting of global ecology of vector transmission enabling Covid-19 to emerge worldwide, by severely uniting the human hosts, vectors and pathogen (Su, et al., 2020). Various studies have shown significant associations between different socio-economic and demographic determinants and prevalence of Covid-19 (Wortham, 2020; Jordan, et al., 2020; Lighter, 2020; Chen, 2020; Zheng, et al. 2020; Chaudhry, 2020; Shaw, et al, 2021). The demographic size, socio-economic characteristics, poor nutrition and associated co-morbidities in India have been serious concerns for long. The emergence of Covid-19 pandemic poses a serious public health challenge in India. In view of this, the understanding of the associated conditions to have caused public health challenge during Covid-19 pandemic has become urgent. This article may have relevance for public health policy interventions as well as for future research in the field for our preparedness for future similar occurrences of disease outbreaks.
Convergence of Demography, Urbanisation, Mobility and Covid-19
Human population growth and economic structure have closely associated with the spread of diseases and public health (Narayan, 2017; McLafferty, 2010). Many of the early pathogens emerged from the diseases of domesticated animals (Dobson & Carper, 1996). The increased population concentration and subsequent mobility among early towns around 5500 BC led to the population threshold to sustain the bacterial and viral infections (Dobson & Carper, 1996). The influenza epidemic in 16th century in Europe and few Asian countries became highly contagious as a result of high population concentration in medieval towns (McNeill, 1976). The majority of the world, including India, until 1950, had experienced low life expectancy and high mortality in the absence of improvements in food production, nutrition, sanitation and hygiene. Nonetheless, along with the expansion of Indian economy, demographic size increased from 360 million in 1950 to 1360 millions in 2019 (United Nations, 2019), causing high population density (382 persons/Km², 2011) (GOI, 2011) (see table 1). Studies reveal that high density of population is positively associated with Covid-19 infection rate (Rocklöv & Sjödin, 2020; Ahmadi, 2020; Copiello, 2020).
The world is rapidly urbanising (4.2 billion) (UN, 2018), and about 29% urban population live in slums (World Bank, 2018). The rising urbanisation is associated with the rise of co-morbidities (Hotez, 2017) and contamination of the environment with pathogens (Coyner, 2002) and has serious implication for public health (Neiderud, 2015; Knowlton 2001; Schmidt & Ostfeld 2001; Patz et al, 2004; WHO, 2010; Alirol, et al, 2011; Saravanan, 2016; Dobson & Carper, 1996). McLafferty (2010) found that rapid industrialisation and poor living and working conditions have neutralized the positive effects of economic development in many developing countries. The rapid growth of cities and consequent increased demand of industrial livestocks have intensified the risk of the emergence and spread of flu pandemic (Davis, 2005). Moreover, the demographic pressure induced land use changes have disrupted local ecologies and escort to increased pathogens and increase human exposure to disease (Mayer, 2000). The spread of the Covid-19 virus and resultant high death rates have been observed in hyper dense megacities across the world (Simon, 2020). The unplanned and haphazard urbanisation (377.1 billion in 2011) in India is highly vulnerable to pandemics (Patidar & Chothodi, 2020; Biswas, 2020; Gani, et al., 2011; Kumar & Quinn, 2012). The rural migrants in urban India live in dilapidated and poverty conditions in (Nova, 2020), poor sanitation (Singhal, et al., 2020). The rising air pollution in the urban areas increase the incidence of lung infection with respiratory diseases such as Pneumonia, Asthma and Chronic Respiratory Disease (CRD) (Phosri, 2019), and Covid-19 infection (Zhu, 2020; Contini, 2020). The global data of Covid-19 pandemic have also made it evident that people with weak respiratory conditions are found to be more susceptible (WHO, 2020). Contrary to the established positive association between urbanisation and pathogens, the rural people, in historic time, also experienced high mortality due to low level of immunity to pathogens (McNeill, 1976) as spread of pathogens reach to rural areas at later age of infection causing high pathogen-induced mortality. The large scale infections and death during second wave of Covid-19 can be attributed to the lower immunity to the Covid-19 in rural India.
Table 1: Population size, growth, density and urbanisation in India, 1901 to 2011

Source: Computed from Census Tables from 1901 to 2011, Census of India (GOI).
In the rapidly transforming economic structure, the global flows of people and goods have expanded and resultantly the potential for the spread of infectious diseases have been amplified (Tatem, et al., 2006; Li, 2005). Human mobility has increased thousand times since 1800 in high income countries (Wilson, 1995). As per UNDESA (2020), 281 million people (3.6 percent of the world population) migrate across international borders each year. The travellers are turned into interactive biological entities to carry microbial genetic substances at different places and times (Wilson, 2003). The hub and spoke structure of the modern transportation networks are becoming a conduit for the transmission of human pathogens (McLafferty, 2010). Covid-19 virus emerged in Wuhan of China's Hubei Province and spread to other parts of the world including India through air travellers (Chaudhry, et al, 2020, Keni, et al., 2020). The travel restriction and lockdowns have slowed down spread of Covid-19 in USA (Paez, 2020; Badr, et al., 2020), U.K. (Hadjidemetriou, et al., 2020), China (Fang, et al., 2020; Kraemer, et al., 2020) and India (Praharaj & Han, 2020). India have nearly 450 million migrants (GOI, 2011) with major share from rural areas who are largely livelihood insecure (Jonathan, 2017; Patidar, 2019) and move to urban areas and constitutes nearly 47 percent of urban population in India (GOI, 2011). The rural to urban migratory linkage is critical determinant of the spread of Covid-19 in urban areas (Biswas, 2020; Patidar, 2020) and in rural areas through reverse migration as evident by (Sharma, 2020).
Figure 1

Source: World Tourism organization (WTO), Yearbook of Tourism Statistics, Compendium of Tourism Statistics and data files, 2021.
Nutrition and Covid-19
In the disease ecology, nutrition of the host may influence the immune system and its susceptibility to viral infection (Gorji & Ghadiri, 2021). The level of nutrition among maternal and children has been decreasing since the Mesolithic period (Lukacs, 2003) due to reduced diversity in diet from a mixture of grains, meat and fruits to a diet dominated only by grains (Cohen & Armelagos, 1984). Micronutrient deficiencies affect nearly 2 billion people worldwide (Allen, et al, 2006) and weaken the immune system and help in developing more virulent strain (Beck, 1997, Beck & Metthews, 2000). The immune system is affected by the specific nutrients or nutrient combinations through the cell activation, alteration in the production of signalling molecules, and gene expression (Valdés-Ramos, et al, 2010). An adequate intake of iron, zinc, and vitamins A, E, B6, and B12 is predominantly vital for the maintenance of immune function (Gleeson, et al., 2004). The protective dietary intakes of key food and nutrients, associated with at least one disease endpoint, have been very limited in India (See table 2). Micronutrient deficiencies decrease the ability to resist infections and are a major public health challenge in developing countries (Katona & Katona, 2008; Samaras, et al. 2013). Studies pointed out the increase in susceptibility of various viral infections among nutritionally deficient individuals (Beck & Matthews, 2000; Ferrari, et al. 2019; Manios, et al, 2018; Kehoe, et al., 2019) including Covid-19 (Naja & Hamadeh, 2020; Calder, 2020; Gorji & Ghadiri , 2021). James, et al (2021), highlighted the importance of adequate nutrition and prevention of obesity and type-2 diabetes to reduce the high risk of Covid-19 outcomes.
Table 2: Dietary intakes of key foods and nutrients in adults aged 25 years and over in India, 2020

Source: Global Burden of Disease, the Institute for Health Metrics and Evaluation, 2020
Note: TMREL: theoretical minimum risk of exposure level (TMREL) represents the optimal dietary intake that minimises risk from all causes of deaths combined.
Co-morbidities and Covid-19
The medical advancement (anti-biotic, immunisation, etc.) have drastically reduced maternal and child death rates from communicable diseases, especially in Lower and Middle Income Countries (LMICs) (Hogan, et al. 2010; You, et al., 2015; Byass, 2016). Six out of the top ten risk factors for mortality worldwide are cardio-metabolic risk factor (high blood pressure, high blood glucose, overweight and obesity, high cholesterol) which are related to lifestyle and behaviour associated with economic development (Narayan, et al., 2010). Over the past few decades, many countries have experienced the increase in average Body Mass Index (BMI), obesity, glucose level and type 2 diabetes (Lukacs & Pal, 2010). The recent research indicated that patients with pre-existing medical conditions especially heart disease, lung disease, diabetes, cancer, and people 60 years and older are more likely to have high severity of coronavirus infection than others (WHO, 2020, WHO, 2019; Yang, 2020; Statista, 2020; Gorji & Ghadiri, 2021; Khan et al., 2021). Studies also indicated that obesity (Jordan, et al., 2020; Lighter, 2020; Chaudhry, et al., 2020; Hajifathalian, 2020; Docherty, et al., 2020) CVD and hypertension (Jordan, et al., 2020; Chen, et al. 2020) are important determinant of Covid-19 infection rate. In addition, male patients with heart injury, hyperglycaemia and high-dose corticosteroid use may have a high risk of Covid induced death (Li, et al, 2020). Nevertheless, children may be less vulnerable to Covid-19 due their more active immunity, stronger respiratory tracts, less exposure to pollution (Lee, et al., 2020) fewer medical disorders, milder disease progression and better prognosis (Ludvigsson, 2020). However, WHO reported that refugee and migrant children, children with deprivation, disabilities, and without parental care and proper shelter are the most vulnerable to Covid-19 (Ludvigsson, 2020). The International Diabetes Federation estimated nearly 73 million diabetes cases (10.4 percent prevalence) between the ages of 20 years and 79 years in 2017 in India (Cho, et al., 2018; IDF, 2019). Half of this population might be unaware of their diabetes status. The undiagnosed diabetes with higher proportions under 50 years of age pose a serious stress on the healthcare system (Tripathy, et al., 2017). Table 3 shows the cases of Diabetes, Asthma, Cancer and Heart Disease among sampled men and women in India. Diabetes is the ninth leading cause of death in India (India Health Metrics, 2015). The recent studies reported that Covid-19 patients had the high prevalence of co-morbidities (Li, et al. 2020; Yang, 2020; Emami, et al. 2020; Hu, et al., 2020; Chen, et al., 2020; Wang, et al., 2020; Singh, et al 2020). Singh & Misra (2020) found that co-morbidities such as hypertension, diabetes, obesity, CVD, CVA, chronic obstructive pulmonary disease, asthma, chronic kidney disease and malignancy are often associated with increase in severity and mortality in patients with Covid-19 in developing countries including India. The diabetes prevalence is the highest in Indian Covid-19 patients compared to other countries (Singh & Misra, 2020). In India, CVD and associated risk factors, including type 2 diabetes, hypertension, and obesity characterize a major and increasing burden of death and disability (Patel, 2011).
Table 3: Health Problems (Self Reported) in India, NFHS- 2015–2016
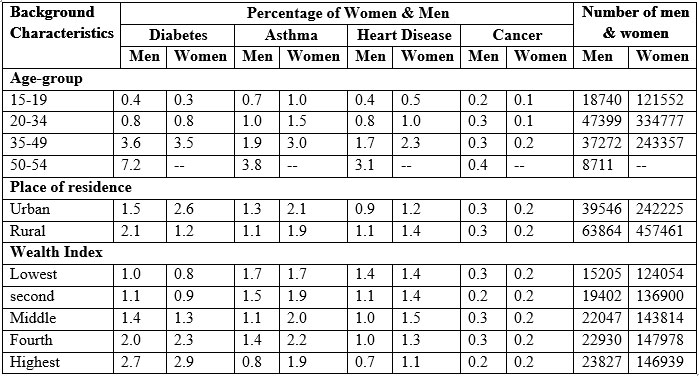
Source: IIPS and National Family Health Survey, India: Key Findings, 2015–2016
Conclusion
Pandemics emerge, spread and controlled through a complex mix of ecological, environmental and socio-economic systems. The population size, urbanisation, mobility, nutrition and co-morbidities and resultant change in ecological set up have heightened the potential for the spread of pandemics. The recent public health challenges caused by the Covid-19 pandemic have caused an urgency to revisit the ecological and pathogenic structure for disease transmission and prevalence. This article aims to highlight the complex association of demographic size, urbanisation, mobility, nutritional status and co-morbidities for their role in the transmission and prevalence of Covid-19 in India. It is found that the convergence of these intertwined issues have aggravated the public health challenges in India during the pandemic. The demographic size, rapid urbanisation, global and local mobility for livelihood, inadequate nutrition and the burden of co-morbidities has undoubtedly heightened the risk of Covid-19 infection and morality. The public health interventions by the governments have reasonably reduced the likely catastrophic outcomes of the pandemic. Nonetheless, Covid-19 is now considered to be an endemic (Phillips, 2021) and in such case it is likely to reappear as an outbreak in future, therefore, there must be an immediate need to enhance nutrition, reduce co-morbidities and develop adequate health infrastructure along with massive vaccination drives for all. The future severity of Covid-19 will depend upon the state’s health monitoring and surveillance, and the future public health response.
References
Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S. J. & Ghanbari, N. 2020. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Science of Total Environment, 729, 138705. (doi:10.1016/j.scitotenv.2020.138705).
Alirol, E. Gétaz, L., Stoll, B., Chappuis, F. & Loutan, L. 2011. Urbanisation of infectious diseases in a globalised world. The Lancet infectious diseases, 11, 131-41. 10.1016/S1473-3099(10)70223-1.
Allen L., de Benoist B., Dary O. & Hurrell R. 2006. Guidelines on food fortification with micronutrients, World Health Organization, Geneva, Switzerland. Accessed from https://www.who.int/publications/i/item/9241594012.
Badr, H. S., Du, H., Marshall, M., Dong, E., Squire, M. M. & Gardner, L. M. 2020. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. The Lancet Infectious Diseases, 20(11), 1247-1254. https://doi.org/10.1016/S1473- 3099(20)30553-3
Beck, M.A., & Matthews, C. 2000. Micronutrients and host resistance to viral infection. Proceedings of the Nutrition Society, 59, 581 - 585.
Beck M. A. 1997. Increased virulence of coxsackievirus B3 in mice due to vitamin E or selenium deficiency. Journal of Nutrition, 127(suppl), 966S–70S. doi: 10.1093/jn/127.5.966S. PMID: 9164275
Binder, S., Levitt, A. M., Sacks, J. J. & Hughes, J. M. 1999. Emerging infectious diseases: Public health issues for the 21st century. Science, 284, 1311–1313
Biswas, P. P. 2020. Skewed Urbanisation and the Contagion, Economic and Political Weekly, 55 (16).
Byass, P. 2016. Child mortality is (estimated to be) falling. Lancet, 388, 2965–67.
Calder, P. C. 2020. Nutrition, immunity and Covid-19. BMJ Nutrition, Prevention & Health, 3:e000085. doi:10.1136/ bmjnph-2020-000085.
Chakraborty I. & Maity, P. 2020. Covid-19 outbreak: Migration, effects on society, global environment and prevention. Science of Total Environment, 728:138882. doi:10.1016/j.scitotenv.2020.138882
Chaudhry R., Dranitsaris G., Mubashir T., Bartoszko J. & Riazi S. 2020. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on Covid-19 mortality and related health outcomes. Eclinicalmedicine, 25, 100464. (doi:10.1016/j.eclinm.2020.100464).
Chen T. et al. 2020. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 368, m1091. (doi:10.1136/bmj.m1091).
Chen Y. M., Gong X., Wang L. & Guo J. 2020. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: a systematic review and meta-analysis. Preprint; medRxiv.
Cho N. H., Shaw, J. E., Karuranga, S., et al. 2018. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Research and Clinical Practice, 138:271–81. https://doi.org/10.1016/j.diabres.2018.02.023
Cohen M. N. & Armelagos, G, J. 1984. Paleopathology at the origins of agriculture. New York: Academic Press.
Contini, D. & Costabile, F. 2020. Does air pollution influence COVID-19 outbreaks? Atmosphere, 11, 377. (doi:10.3390/atmos11040377).
Copiello, S. & Grillenzoni, C. 2020. The spread of 2019-nCoV in China was primarily driven bypopulation density. Comment on ‘Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China’ by Zhu et al. Science of Total Environment, 744, 141028. doi:10.1016/j.scitotenv.2020.141028).
Coyner, D.F. et al. 2002. Epizootiology of Eustrongylides ingotus in Florida: distribution, density, and natural infections in intermediate hosts. J. Wildl. Dis. 38, 483–499.
Daszak, P.,Cunningham, A. A. & Hyatt, A. D. 2000. Emerging infectious diseases of wildlife — threats to biodiversity and human health. Science 287, 443–449.
Davis, M. 2005. The Monster at Our Door: The Global Threat of Avian Flu. New York, NY: Owl Books.
Diamond, J. 2002. Evolution, consequences, and future of plant and animal domestication. Nature, 418, 34–41.
Diamond, J. 1997. Guns, Germs, and Steel: the Fates of Human Societies. Norton, New York, 2.
Dobson, A. P. and Carper, E. R. 1996. Infectious Diseases and Human Population History. BioScience, 46(2).
Docherty A. B., Harrison E. M., Green C. A., Hardwick, H., Pius R., Norman L., et al. 2020. Features of 20133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohortstudy. BMJ 369:m1985. https://doi.org/10.1136/bmj.m1985.
Emami A, Javanmardi F, Pirbonyeh N, Akbari A. 2020. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med, 8(1), e35.
Fang, H., Wang, L., Yang, Y. 2020. Human Mobility Restrictions and the Spread of the Novel Coronavirus (2019-nCoV) in China. Cambridge, MA. https://doi.org/10.3386/w26906
Ferrari D, Lombardi G, Strollo M, Pontillo M, Motta A, Locatelli M. 2019. Association between solar ultraviolet doses and vitamin D clinical routine data in European mid-latitude population between 2006 and 2018. Photochem Photobiol Sci, 18, 2696–706.
Gani S. R., Ali, S. T. & Kadi, A. S. 2011. The transmission dynamics of pandemic influenza A/ H1N1 2009–2010 in India, Current Science, 101(8). pp. 1065–1072.
Gleeson M., Nieman D. C. & Pedersen B. K. 2004. Exercise, nutrition and immune function. Journal of Sports Science, 22, 115–25.
Gorji A. and Ghadiri, M. K. 2021. Potential roles of micronutrient deficiency and immune system dysfunction in the coronavirus disease 2019 (COVID-19) pandemic. Nutrition, 82 111047. https://doi.org/10.1016/j.nut.2020.111047.
Government of India. 2011. Data on Workers (B-Series), Office of the Registrar General & Census Commissioner, India, Government of India, New Delhi.
Government of India. 2011. Migration Tables (D-Series), Office of the Registrar General & Census Commissioner, India, Government of India, New Delhi.
Government of India. 2011. Primary Census Abstract, Office of the Registrar General & Census Commissioner, India, Government of India, New Delhi.
Hadjidemetriou, G.M., Sasidharan, M., Kouyialis, G., Parlikad, A.K. 2020. The impact of government measures and human mobility trend on COVID-19 related deaths in the UK. Transportation Research Interdisciplinary Perspectives 6, 100167. https://doi.org/10.1016/j.trip.2020.100167
Hajifathalian K, Kumar S, Newberry C, et al. 2020. Obesity is associated with worse outcomes in COVID-19: analysis of early data from New York city. Obesity, https://doi.org/10.1002/oby.22923
Hogan, M.C., Foreman, K.J., Naghabi, M., Ahn, S.Y., Wang, M., Makela, S.M., et al. 2010. Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet, 375:1609–23.
Hotez, P. J. 2017. Global urbanization and the neglected tropical diseases. PLoS Neglected Tropical Diseases, 11(2). https://doi.org/10.1371/journal.pntd.0005308.
Hu Y, Sun J, Dai Z, Deng H, Xin L, Huang Q, et al. 2020. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. Journal of Clinical Virology, 127:104371.
IDF, 2019. IDF diabetes atlas – 2019, International Diabetes Federation. https://diabetesatlas. org/ [Accessed 2019 Apr 26].
India State-Level Disease Burden Initiative Collaborators, 2017. Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet, 390 (10111):2437-2460. https://doi.org/10.1016/S0140-6736(17)32804-0
India: Health Metrics 2015. Institute for health metrics and evaluation. http://www. healthdata. org/ india
International Institute for Population Sciences. 2016. National Family Health Survey, India: Key Findings, Available online: http://rchiips.org/NFHS/factsheet_NFHS-4.shtml (accessed on 20 September 2019).
Jonathan C. 2017. Urbanisation, Growth, and Development: Evidence from India, World Bank, Washington, DC. Retrieved 26 May 2020 from, https://www.gov.uk
Jones, K. E., Patel, N. G., Levy, M. A., Storeygard, A., Balck, D., Gittleman J. L., and Daszak P. 2008. Global Trends in Emerging Infectious Diseases. Nature, 451(21), 990-994.
Jordan R.E., Adab P. & Cheng K.K. 2020. Covid-19: risk factors for severe disease and death. BMJ, 68, m1198 (doi:10.1136/bmj.m1198).
Katona P. & Katona-Apte J. 2008. The interaction between nutrition and infection. Clinical infectious diseases, 46:1582–8. https://doi.org/10.1086/587658.
Kehoe L., Walton J. & Flynn, A. 2019. Nutritional challenges for older adults in Europe: current status and future directions. Proceedings of the Nutrition Society, 78: 221–33.
Keni, R., Alexander, A., Nayak, P. G., Mudgal, J., & Nandakumar, K., 2020. Covid-19: Emergence, Spread, Possible Treatments, and Global Burden. Frontiers in Public Health, 8:216. doi: 10.3389/fpubh.2020.00216
Khan, W., Hussain, A., Khan, S. A., Al-Jumailey, M., Nawaz, R. & Liatsis, P. 2021. Analysing the impact of global demographic characteristics over the COVID-19 spread using class rule mining and pattern matching. Royal Society Open Science,. 8: 201823. https://doi.org/10.1098/rsos.201823.
Knowlton, K. 2001. Urban history, urban health. American Journal of Public Health, 91(12), 1944–1946. https://doi.org/10.2105/ajph.91.12.1944
Kraemer, M.U.G., Yang, C.H., Gutierrez, B., Wu, C.H., Klein, B., Pigott, D.M., du Plessis, L., Faria, N.R., Li, R., Hanage, W.P., Brownstein, J.S., Layan, M., Vespignani, A., Tian, H., Dye, C., Pybus, O.G. & Scarpino, S. V. 2020. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science, 368, 493–497. https://doi.org/10.1126/science.abb4218.
Krause, R. M. 1992. The origin of plagues: old and new. Science, 257, 1073-1078.
Kumar, S. & Quinn, S. C. 2012. Existing health inequalities in India: informing preparedness planning for an influenza pandemic, Health Policy and Planning, 27(6), p. 516.
Lee, P. I., Hu, Y. L., Chen, P. Y., Huang, Y. C. & Hsuehe, P. R. 202). Are children less susceptible to Covid-19? Journal of Microbiology, Immunology and Infection, 53, 371–372. doi:10.1016/j.jmii.2020.02.011.
Li, B., Yang, J., Zhao, F., et al. 2020. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clinical Research in Cardiology, 109(5):531e8. https://doi.org/10.1007/s00392-020-01626-9.
Li, Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y. & Xing X. 2020. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New England Journal of Medicine, (January 29, 2020) doi: 10.1056/NEJMoa2001316.
Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, et al. 2005. Bats are natural reservoirs of SARS-like coronaviruses. Science, 310, 676-9.
Li X, Xu S. et al. 2020. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. Journal Allergy Clinical Immunology, 146, 110–118. (doi:10.1016/j.jaci.2020.04.006)
Lighter, J., Phillips, M., Hochman, S., Sterling, S., Johnson, D., Francois, F. & Stachel, A. 2020. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission. Clinical Infectious Diseases, 71(15), 896-897. https://doi.org/10.1093/cid/ciaa415
Ludvigsson, J. F. 2020. Systematic review of COVID- 19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica. 109, 1088–1095. https://doi.org/10.1111/apa.15270
Lukacs, J. R. & Pal, J. N. 2003. Skeletal variation among Mesolithic people of the Ganga plains: New evidence of habitual activity and adaptation to climate. Asian Perspectives, 42(2), 329–351.
Manios, Y., Moschonis, G., Lambrinou, C.P., Tsoutsoulopoulou, K., Binou, P., Karachaliou, A., et al. 2018. A systematic review of vitamin D status in southern European countries. Europen Journal of Nutrition, 57, 2001–2036. https://doi.org/10.1007/s00394-017-1564-2.
Mayer, J. D. 2000. Geography, ecology and emerging infectious diseases. Social Science and Medicine, 50(7-8), 937-52. doi: 10.1016/s0277-9536(99)00346-9.
McLafferty, S. 2010. Placing Pandemic : Geographical Dimensions of vulnerability and spread. Eurasian Geography and Economics, 51(2), 143-161. https://doi.org/10.2747/1539-7216.51.2.143.
McNeill, W. H. 1976. Plagues and Peoples, Anchor, Garden City.
Morens, D. M., Folkers, G. K. & Fauci, A. S. 2004. The challenge of emerging and reemerging infectious diseases. Nature, 430, 242–249.
Morse, S. S. 1993. Examining the Origins of Emerging Viruses. In: Morse S.S., ed. Emerging Viruses. New York: Oxford University Press, pp. 10–28.
Naja, F. and Hamadeh, R. 2020. Nutrition amid the COVID-19 pandemic: a multi-level framework for action. European Journal of Clinical Nutrition, 74:1117–1121. https://doi.org/10.1038/s41430-020-0634-3.
Narayan K. M. V., Ali, M. K. & Koplan, J. P. 2010. Global noncommunicable diseases: Where worlds meet. N Engl J Med, 363:1196–8.
Narayan, V. K. M. 2017. Public Health Challenges for the 21st Century: Convergence of demography, economics, environment and biology: Nalanda Distinguished Lecture. The National Medical Journal of India, 30(4), 219-223.
Wolfe, N. D., Dunavan, C. P. & Diamond, J. 2007. Origins of major human infectious diseases. Nature, 447, 279-283. doi:10.1038/nature05775.
Neiderud, C. J. 2015. How urbanization affects the epidemiology of emerging infectious diseases, Infection Ecology & Epidemiology, 5:1, DOI: 10.3402/iee.v5.27060.
Nova, C. 2020. Covid-19 and the water crisis in India: a wakeup call for clean water. Smart water magazines, Retrieved 26 May 2020 from, https://smartwatermagazine.com
Paez, A. 2020. Using Google Community Mobility Reports to investigate the incidence of COVID19 in the United States. Transport Findings 12976. https://doi.org/10.32866/001c.12976
Patel V., Chatterji S., Chisholm D., et al. 2011. Chronic diseases and injuries in India. Lancet, 377(9763). doi:10.1016/S0140-6736(10)61188-9
Patidar, H. 2018. Livelihood Security in Rural India: Reflections from Some Selected Indicators. Forum for Development Studies, 46 (1). https://doi.org/10.1080/08039410.2018.1519517.
Patidar, H., & Chothodi, S. 2020. Revisiting Urbanisation Pattern amid COVID-19 Pandemic in India. Space and Culture, India, 8(2), 4-24. https://doi.org/10.20896/saci.v8i2.1008.
Patz, J. A. et al. 2004. Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence. Environ. Health Perspectives. 112, 1092–1098 (2004).
Phillips, N. 2021. The coronavirus is here to stay — here’s what that means. Nature, 16 February 2021. https://www.nature.com/articles/d41586-021-00396-2
Phosri A, Ueda K, Phung VLH, Tawatsupa B, Honda A, Takano H. 2019. Effects of ambient air pollution on daily hospital admissions for respiratory and cardiovascular diseases in Bangkok, Thailand. Science of Total Environment. 651, 1144–1153. doi:10.1016/j.scitotenv.2018.09.183)
Praharaj, S. And Han, H. A. 2020. longitudinal study of the impact of human mobility on the incidence of COVID-19 in India. MedRxiv: The Preprint server of health science. BMJ Yale. doi: https://doi.org/10.1101/2020.12.21.20248523
Rocklöv, J. & Sjödin, H. 2020. High population densities catalyse the spread of COVID-19. Journal of travel medicine, 27(3), taaa038. https://doi.org/10.1093/jtm/taaa038
Samaras, D., Samaras, N., Lang, P.O., Genton, L., Frangos, E., Pichard, C. 2013. Effects of widely used drugs on micronutrients: a story rarely told. Nutrition, 29:605–10.
Saravanan, V. S., Idenal, M. A., Saiyed, S., Saxena, D. & Gerke, S. 2016. Urbanization and human health in urban India: institutional analysis of water-borne diseases in Ahmedabad, Health Policy and Planning, 31(8), 1089–1099, https://doi.org/10.1093/heapol/czw039
Schmidt, K,A. & Ostfeld, R.S. 2001. Biodiversity and the dilution effect in disease ecology. Ecology, 82:609–619.
Sharma, N. C. 2020. Rural India is the new covid-19 flashpoint amid migrant influx. Livemint, https://www.livemint.com/news/india/rural-india-is-the-new-covid-19-flashpoint-amid-migrant-influx-11590608606400.html. 28/05/2020. Accessed on 02 June 2020.
Shaw A. K., White, L. A., Michalska-Smith, M., Borer, E. T., Craft, M. E., et al. 2021. Lessons from movement ecology for the return to work: Modeling contacts and the spread of COVID-19. PLOS ONE 16(1): 0242955. https://doi.org/10.1371/journal.pone.0242955
Simon, D. 2020. Cities are at centre of coronavirus pandemic –understanding this can help build a sustainable, equal future, The Conversation, 23 April 2020.
Singh, A,K., Gilles, C., Singh, R. et al. 2020. Prevalence of comorbidities and their association with mortality in patients with COVID -19: a Systematic Review and Meta-analysis. Diabetes Obesity & Metabolism. https://doi.org/10.1111/dom.14124; June 23 2020.
Singh, A.K. A. & Misra A. 2020. Impact of COVID-19 and comorbidities on health and economics:Focus on developing countries and India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 14. 1625-1630. https://doi.org/10.1016/j.dsx.2020.08.032.
Singhal, S., Matto M. & Parsad J. 2020. COVID-19: Hits & misses of Centre’s advisory on water supply, sanitation: A review of MoHUA April, 2020 advisory on safe management of water supply and sanitation. https://www.downtoearth.org. 18/05/2020. Accessed on 16 June 2020.
Smolinski, M. S., Hamburg, M. A. & Lederberg, J. 2003. Microbial Threats to Health: Emergence, Detection, and Response (National Academies Press, Washington DC, 2003).
Statista 2020. Distribution of coronavirus cases in Italy as of March 25, 2020. Available at: https://www.statista.com/search/?q=Distribution§of§Coronavirus§cases&Search=&qKat=search. Accessed May 3, 2020.
Su, D., Chen, Y., He, K., Zhang, T., Tan, M., Zhang, Y. & Zhang, X. 2020. Influence of socio-ecological factors on COVID-19 risk: a cross-sectional study based on 178 countries/regions worldwide. Pre-print. doi: https://doi.org/10.1101/2020.04.23.20077545
Tatem, A. J., Rogers, D. J. & Hay, S. I. 2006. Global Transport Networks and Infectious Disease Spread. Advances in Parasitology. https://doi.org/10.1016/S0065-308X(05)62009-X.
Taylor, L. H., Latham, S. M. & Woolhouse, M. E. J. 2001. Risk factors for human disease emergence. Philosophical Transaction of Royal Society, B, 356, 983–989. https://doi.org/10.1098/rstb.2001.0888
The Copenhagen Consensus project on hunger and malnutrition Hunger and malnutrition. 2012. Available at: https://www.copenhagenconsensus.com/sites/default/files/hungerandmalnutrition.pdf. Accessed May 3, 2020.
Tripathy J. P., Thakur, J. S., Jeet, G. & Jain, S. 2017. Prevalence and determinants of comorbid diabetes and hypertension: Evidence from non communicable disease risk factor STEPS survey, India. Diabetes Metabolic Syndrome: Clinical Research & Reviews, 11 (Suppl), S459-S465. doi: 10.1016/j.dsx.2017.03.036.
United Nation. 2018. 68% of the world population projected to live in urban areas by 2050, says UN. Department of Economic and Social Affairs.
United Nation. 2019. World Population Prospects- 2019 Highlights, Department of Economic and Social Affairs Population Division, accessed from https://population.un.org/wpp/Publications/Files/WPP2019_Highlights.pdf
United Nations. 2020. International Migration 2020 Highlights. https://www.un.org/en/desa/international-migration-2020-highlights
Valdés-Ramos R, Martínez-Carrillo BE, Aranda-González II, Guadarrama AL, Pardo-Morales RV, Tlatempa P, et al. 2010. Diet, exercise and gut mucosal immunity. Proc Nutr Soc. 69:644–650.
Wang, B., Li, R., Lu, Z., Huang, Y. 2020. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging 2020;12:6049e57. https://doi.org/10.18632/aging.103000.
Weiss, R. A. & McMichael, A. J. 2004. Social and environmental risk factors in the emergence of infectious diseases. Nature Med. 10, S70–S76.
Wilson, M. 2003. The Traveler and Emerging Infections: Sentinel, Courier, Transmitter,” Journal of Applied Microbiology, 94, 1S–11S.
Wilson, M. 1995. Travel and the Emergence of Infectious Disease, Emerging Infectious Diseases, 1, 1:39–146.
Word Bank 2018. Word Bank Data. Retrieved 16 June 2020 from https://data.worldbank.org
World Bank. Population living in Slums. https://data.worldbank.org/indicator/EN.POP.SLUM.UR.ZS. accessed on 30.08.2021
World Health Organization 2010. Hidden cities: unmasking and overcoming health inequities in urban settings. Kobe, Japan: World Health Organizaiton.
World Health Organization. Coronavirus disease 2019 (COVID-19) situation report—124. Available at: https://www.who.int/docs/default-source/corona viruse/situation-reports/20200523-covid-19-sitrep-124.pdf?sfvrsn=9626d639_2. Accessed 24 May2020.
World Health Organization. Coronavirus disease 2019 (COVID-19). 2020. situation report, 51. World Health Organization, Geneva.
World Health Organization. 2019. Facts: urban settings as a social determinant of health. Available from: http://who.int/social_determinants/publications/urbanization/factfile/en/
World Health Organization. Report of the WHO_China Joint Mission on Coronavirus Disease 2019 (COVID-19), 2020. Available at: https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirusdisease-2019-(covid-19). Accessed May 3, 2020.
World Tourism organization, Yearbook of Tourism Statistics, Compendium of Tourism Statistics and data files. Accessed on 30.07.2021. https://data.worldbank.org/indicator/ST.INT.ARVL?locations=IN
Wortham J. M. et al. 2020. Characteristics of persons who died with COVID-19—United States. Centre for Disease Control Prevention. Morbidity and Mortality Weekly Report, 69(28), 923–929. (doi:10.15585/mmwr.mm6928e1)
Yang, J,, Zheng ,Y,, Gou, X., Pu, K., Chen, Z., Guo, Q., et al. 2020. Prevalence of comorbidities and its effect in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International Journal of Infectious Disease, 94, 91-95.
Hu, Y., Sun, J., Dai, Z., Deng, H., Li, X., Huang, Q., Wu, Y., Sun, L., & Xu, Y. 2020. Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology, 127, 104371. https://doi.org/10.1016/j.jcv.2020.104371
You, D., Hug, L., Ejdemyr, S., Idele, P., Hogan, D., Mathers, C., et al. 2015. United Nations Interagency Group for Child Mortality Estimation (UN IGME). Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet, 386, 2275–86.
Zheng, Z. et al. 2020. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. Journal of Infection, 81(2), e16–e25. (doi:10.1016/j.jinf.2020.04.021)
Wang, Z., Yang, B., Li, Q., Wen, L. & Zhang, R. 2020. Clinical Features of 69 Cases With Coronavirus Disease 2019 in Wuhan, China, Clinical Infectious Diseases, 71(15), 769–777. https://doi.org/10.1093/cid/ciaa272.
Zhu, Y., Xie, J., Huang, F., Cao, L. 2020. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Science of Total Environment, 727, 138704. (doi:10.1016/j.scitotenv.2020.138704).
(Hemant Patidar, Assistant Professor, Department of General & Applied Geography, School of Applied Sciences, Dr. Harisingh Gour Vishwavidyalaya, Sagar (M.P.) India)
Disclaimer: The opinions expressed in this article are the personal opinions of the author. The facts and opinions appearing in the article do not reflect the views of Indiastat and Indiastat does not assume any responsibility or liability for the same.
indiastat.comJune, 2022
socio-economic voices
